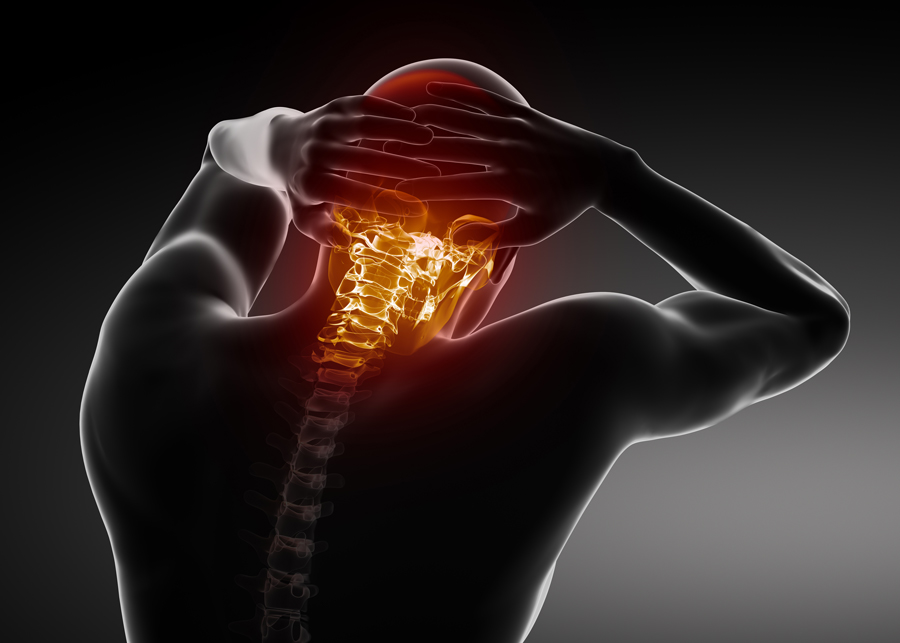
Headaches and neck pain: The impact of cervical anatomy
Headaches happen for many different reasons. Stress, tiredness, eyestrain, trauma, or even the weather, all are examples of factors that can cause headaches.
Headaches are not necessarily rooted in the head. Some originate from problems with the nerves, muscles or bones in the neck; these are called cervicogenic headaches. About 15–20% of all headaches are cervicogenic. They affect around 4% of the general population and typically result in pain on one side of the head or face. It is a steady pain that stays in one spot and can last for hours or days. The headache can be associated with a stiff neck or even neck pain.

Many things can cause a cervicogenic headache, and sometimes there is no way to figure out exactly what it was. A cervicogenic headache can come from a sudden movement of the neck. It may also occur when the neck remains in the same position for long periods of time, for example while sitting at a desk for hours at work, or when falling asleep in an awkward position: a wrong posture, such as pushing the chin forward (which moves the head out in front of the body), can put extra weight on the neck and base of the skull, and trigger a cervicogenic headache. A fall, an injury, a fracture, a tumour, arthritis, or anything that compresses the nerves in the neck can also be responsible for a cervicogenic headache.
While many potential causes are known, the exact mechanisms by which cervicogenic headaches are caused are still not clear.
To understand this, Dr Sillevis and his team explored the anatomical relationship between different structures in the neck because a thorough knowledge of head and neck anatomy is needed to understand how cervicogenic headaches happen and how to treat them.
Spine and spinal cord
Running down from skull to lower back, the spine is subdivided into different regions: the cervical spine, in the neck, is made of seven bones named vertebrae. Twelve vertebrae compose the thoracic spine, and five form the lumbar spine in the lower back. Sacrum and coccyx constitute the lower end of the spine. The cervical spine is the one that is of interest here.
Between each vertebra, an intervertebral disc forms a cartilaginous joint that allows slight movement of the vertebrae, acts as a ligament to hold the vertebrae together, and functions as a shock absorber for the spine.
A thorough knowledge of head and neck anatomy is needed to understand how cervicogenic headaches happen
and how to treat them.
A hollow opening in the centre of the spinal column forms a canal that houses and protects the spinal cord, which is part of the central nervous system. Inside the canal, the spinal cord is surrounded by three protective envelopes named, from the inside to the outside, the pia mater, the arachnoid and the dura mater. The area between the dura and the inner surface of the bone is called the epidural space.

The cervical spine
The neck is unique in that it supports the weight of the head and also allows diverse movements, such as turning the head from side to side, nodding, and looking up and down. The upper cervical spine is the most mobile section of the entire spine: out of the seven vertebrae, labelled from C1 to C7, C1 (also called the atlas) and C2 (also called the axis) contribute to more than 50% of the total rotation, flexion (bending forward) and extension (bending backward) of the neck.
The seven vertebrae also protect the spinal cord as well as the spinal nerves that exit the spine between each vertebra.
The spinal nerves
The spinal cord and nerves connect the brain with other parts of the body, providing sensation (feeling) and motor function (movement) to each of them. Spinal nerves exit the spine in pairs: one nerve exits on the left side and one on the right.
In the neck, the eight pairs of cervical spinal nerves, numbered to correspond to the level in the cervical spine, from C1 to C8, innervate the upper body: C1, C2 and C3 enable sensation and movement of the head and neck. Sensation and movement of the shoulders depend on C4 and C5. C6, C7 and C8 innervate arms and hands; for example, C6 provides sensation down to the thumb, C7 to the middle finger, and C8 to the little finger.
Supporting the spine
Ligaments, tendons and muscles are soft but strong tissues that help support the cervical spine as well as the entire spinal column by limiting excessive movement. Among these supporting structures, the nuchal ligament spans the cervical spine from the base of the skull to the seventh cervical vertebra in the lower part of the neck.
Meningovertebral ligaments can be found within the epidural space (the area between the dura that protects the spinal cord and the inner surface of the vertebrae). All along the length of the vertebral column, these fibrous connections anchor the spinal cord in the spinal canal by attaching the outer surface of the dura to the inner borders of the canal.
Muscles also play a major part in supporting the spine. The three main muscles found in the upper cervical region are named Rectus Capitis Posterior Major, Rectus Capitis Posterior Minor, and the Obliquus Capitis Inferior.
Myodural bridges are connections made of soft tissue that link these muscles with the dura. Myodural bridges play a role in protecting the dura during motion and preventing compression of the spinal cord.
A cadaver study
In patients with upper cervical dysfunction such as cervicogenic headaches, there appears to be a relationship between the movement or position of the spine and the intensity of headaches. To know more about this, Dr Sillevis designed a study that aimed to gain insight into how the upper cervical spine, especially the muscles, ligaments and soft tissue, might be connected to the central nervous system.
Muscle tone and position of the head and neck could result in a pulling effect of the dura that may cause neural tension.
Dissection of seven cadavers allowed him to study cervical anatomy. More specifically, Dr Sillevis aimed to explore the soft tissue connections between the muscles of the upper cervical region, the ligaments and the dura mater, and to examine the position of the spinal cord during motion of the upper cervical region. A better understanding of these anatomical relationships and response to movement might help to explain how cervicogenic headaches happen and how to treat them.
Explaining cervicogenic headaches
The upper cervical spine is a very complex anatomical region. Dr Sillevis was able to demonstrate that structures in the upper cervical region are highly interconnected through ligaments, myodural bridges and other soft tissue. The epidural space contains many connective tissues (made of collagen) that merge and blend together regardless of their origination. The muscles in the back of the neck and the nuchal ligament both have direct connections with the dura. These connections suggest that muscle tone and position of the head and neck could result in a pulling effect of the dura that would cause neural tension. This could explain why patients complain about neck pain or headache.

Dr Sillevis was also able to demonstrate that motion of the upper cervical region impacts the position of the spinal cord: when the C1 vertebra rotates, the spinal cord is pulled in the same direction within the spinal canal. If muscle tone is already pulling the spinal cord in the opposite direction, this can increase neural tension and contribute to additional complaints and symptoms in patients.
Clinical implications
This work has important clinical consequences. Notably, the collagenous connections observed by Dr Sillevis between the nuchal ligament, the myodural bridges and the dura, and the movement of the first vertebra affecting the spinal cord position within the canal offers clinicians options to identify cervical dysfunctions and treat patients with headaches and neck pain far more effectively.
Personal Response
What is next for your research?
<> The next step in my research is looking clinically at the relationship between the position of atlas and the intensity and presence of the cervicogenic headaches and how we can reliably establish a positional default from atlas. A retrospective study is underway to explore this relationship. We will continue with a cadaver study and further assess the effect of neural tension on the spinal cord position.
Besides the research efforts to better understand the anatomical and clinical relevance of the upper cervical spine in headaches and neck pain, another research focus uses the brain-computer interface to evaluate the direct effect of physical therapy interventions on brain activity (based on brainwaves). Several studies are underway aiming to map normal brainwave activity and the response to interventions. The objective is to better determine which intervention is optimal for a patient based on their specific brainwave pattern.