New possibilities: Same-day surgery for trochlear dysplasia
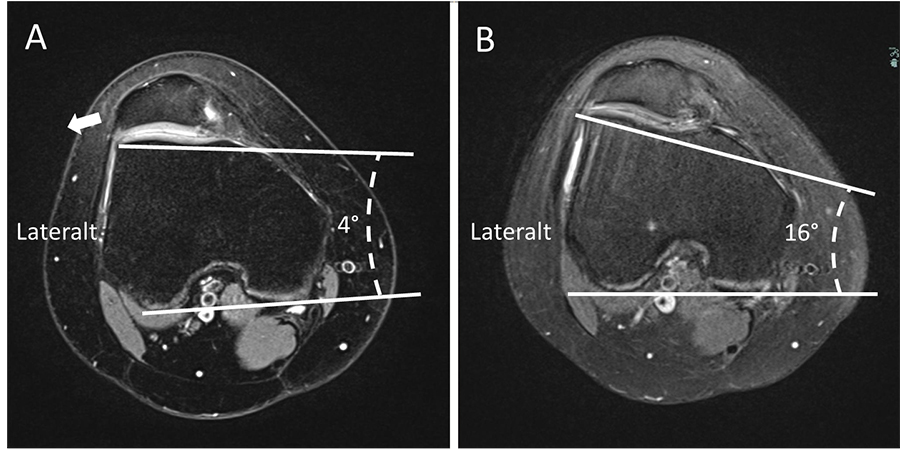
The trochlea of the knee is a groove at the end of the femur (thigh) bone in which the patella sits. The walls of the groove provide the patella with stability, as it moves back and forth within the groove as the knee bends and straightens. Trochlear dysplasia describes a condition when the shape of the trochlea groove is abnormal (too shallow or uneven) and causes dislocation of the patella, also known as patellofemoral instability. It can also lead to chronic patellofemoral pain or artrosis. This may be caused by an injury to the knee, pushing the patella completely out of the trochlear groove (dislocation), or a chronic instability where the patella slides partially out of the trochlea (subluxation). Since it can happen at any time, without a preceding injury, it makes the affected patient anxious and concerned.
In the early 1990’s, researchers reported that up to 90% of patellofemoral instability is caused by trochlear dysplasia. Initially treatment consists of rest, use of crutches or braces, followed by physiotherapy. In cases where the patella instability is affecting patient’s lifestyle, surgery is warranted. The procedure to restore the normal trochlear anatomy is an open surgery called a trochleoplasty. The aim is to deepen the trochlear groove, so the patella sits back into the correct configuration.

Experimenting with the procedure
Dr Lars Blønd began performing open trochleoplasty surgery in 2005, after learning the open technique from Dr Philip Schöttle. With extensive experience, Dr Blønd taught anthroscopy to surgeons in training, using cadavers for his demonstrations. This led to the opportunity to experiment with the procedure and to develop portals, shavers, and fixation techniques to improve surgery in cooperation with the company Arthrex. Since the risk of infection, pain, and arthrofibrosis (build-up of scar tissue around the joint) is high with the traditional open surgery, this research was highly important. Finally, a technique was perfected, as Dr Blønd’s team developed a minimally invasive arthroscopic (joint) procedure which would avoid surgically opening the knee.
The first patient left hospital the same day and soon after, he wanted the other knee operated on as well.
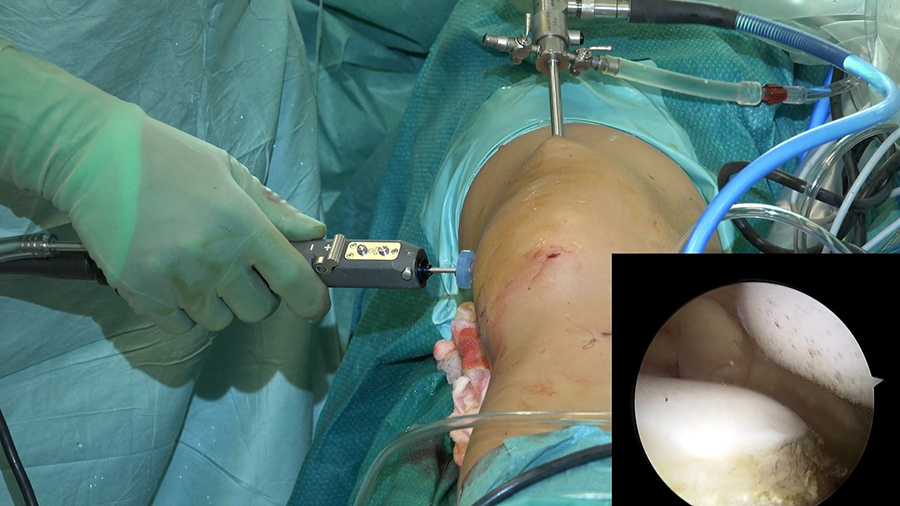
Arthroscopy uses an arthroscope (a pinhole instrument that has a camera at one end, allowing visualisation of the internal anatomy) inserted into the body through a small incision which allows faster recovery and less pain.
Dr Blønd recalls, “we managed to come up with a result that I found reliable and safe to try out with the first patient”. In a 2009 research paper, with the help of Dr Philip Schöttle, Dr Blønd presented the first results using this new technique, called arthroscopic deepening trochleoplasty (ADT).

The ADT procedure
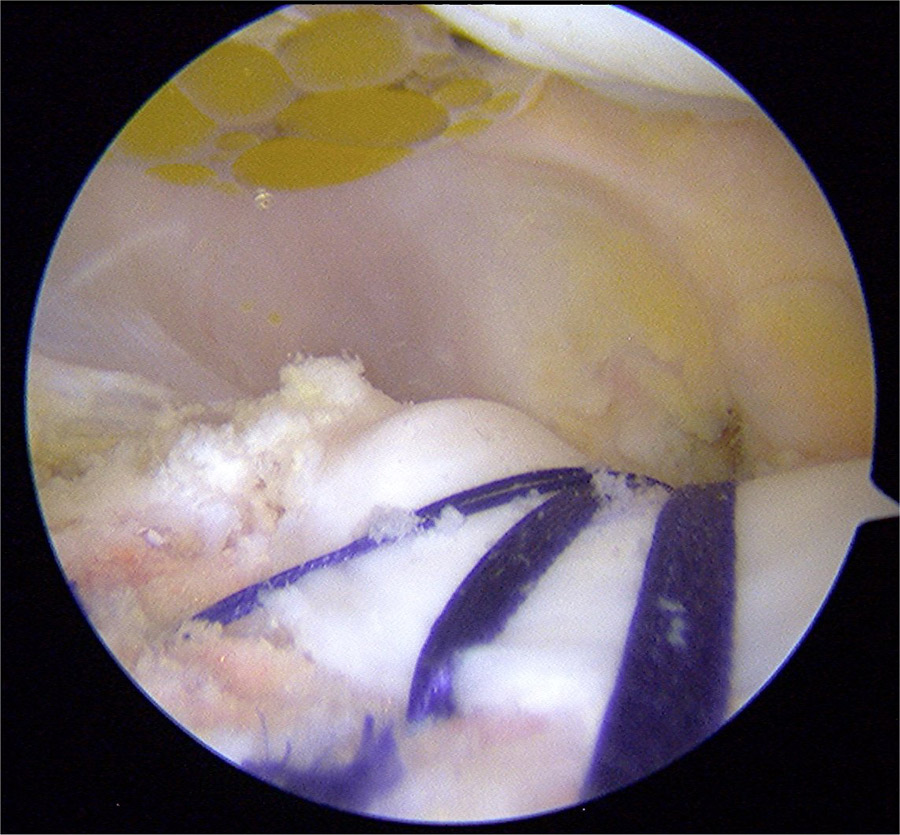
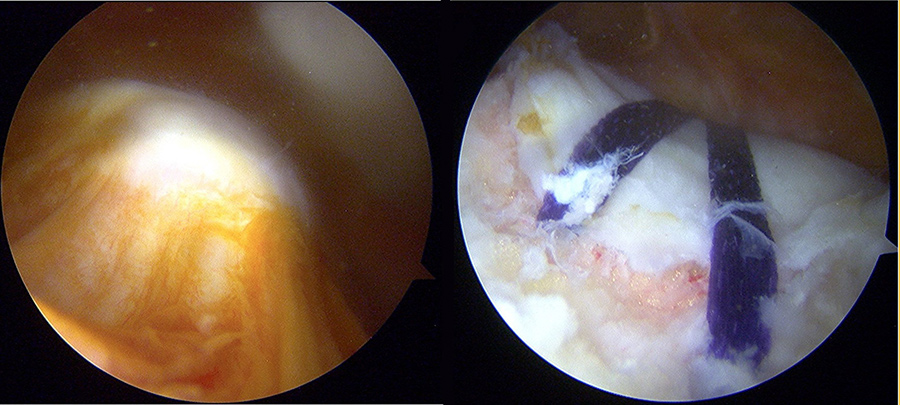
In this study, Dr Blønd and colleagues enrolled patients who had had two or more patellar dislocations as well as trochlear dysplasia. The paper describes the surgical technique: two small incisions are made (known as lateral and proximal) to allow space and to give a better view of the joint. An additional incision proximal to the lateral border of the trochlear is made and a canula is placed here. From this portal, synovial fluid proximal to the trochlear is removed until the outer (cortical) surface of the bone is exposed. The team then use a 4 mm round burr shaver to cut between the bone and cartilage, releasing what is known as a ‘cartilaginous flake’. The burr shaver is used, steadily switching between the different incision sites to slowly carve a curve into the trochlear.
Once the correct shape and depth are achieved, as per a normal anatomy, the cartilage flake is then re-fixated using four 3.5 mm knotless suture anchors and eyelet. A hole is predrilled distal to the hinge of the cartilage flake and the anchor loaded with a 3 mm absorbable tape is fixed into the hole to hold the tape and suture in place. Additional anchors are then placed via the other incision, proximal to the border of the cartilage flake to hold down the flake in the correct position.
Following the surgery, all the patients left hospital the next morning. As a result of the new surgical technique, all the patients were able to achieve full weight bearing from the first post-operative day, and are allowed range of motion without a brace or knee immobiliser. Moreover, 3 months after surgery, all patients were negative for patellar apprehension sign (a physical examination indicating the absence or presence of patellar instability).
The researchers explain: “The most important finding of this study is that the deepening trochleoplasty can be done using an arthroscopic technique and that the procedure seems to be less painful compared to the open procedure.” Furthermore, in comparison to the open surgery, Dr Blønd’s technique has the advantage of faster mobilisation post-operatively, lower risk of arthrofibrosis, and reduced scar formation.
As a result of the new surgical technique, all patients were able to achieve full weight bearing from the first post-operative day.
Medial patellofemoral ligament reconstruction
In a later paper (2013), the researchers describe a follow-up study reporting the clinical outcomes of patients having ADT followed by medial patellofemoral ligament reconstruction (MPFLR). The authors explain, “The ADT alone only provides minor stability for the patella in full extension, contrary to the MPFLR technique, which provides stability in the whole range of movement.” The follow-up examinations, undertaken a minimum of 12 months after the surgery, revealed no complications, re-dislocations or arthrofibrosis in 29 of the knees that underwent the technique. The research concluded that ADT in combination with MPFLR was found to be a safe and reproducible procedure and is superior to the open technique.

As Dr Blønd performed more ADT surgeries, he later made a slight modification to the original technique by omitting the use of the superior lateral cannula, as he found that its use was not necessary. The indications for the procedure were also expanded to patients with degenerative changes in the trochlea region and those with severe trochlea dysplasia without instability suffering from chronic severe anterior knee pain. In a 2017 paper, Dr Blønd and colleagues report the first case studies of two patients suffering from years of chronic anterior knee pain and trochlear dysplasia that were successfully treated by ADT.
Since performing the first of these procedures in 2008, Dr Blønd tells us that the procedure is now internationally recognised and has been rolled out in 11 countries. He recalls: “The first patient was thoroughly informed and more than ready. Surprisingly, he left the hospital the same day and soon after, he wanted the other knee operated as well.” The minimally invasive technique has attracted patients from as far as Hawaii, with a former patient, Kenneth Chan, sending a follow-up video 1 year after having the surgery showing him jump over a metre-high hurdle.
The studies conducted so far provide evidence that ADT is a more advantageous procedure compared to open trochleoplasty. It has proved to be faster, technically easier, and can be performed as same-day surgery which makes it more economical due to a much shorter time in hospital. For the open surgery, at least 3-4 days hospital stay is required. Many of Dr Blønd’s patients have testified to the efficacy of the treatment, and Dr Blønd has shared an interesting video made by his son, Asker Blønd, that covered a Trochleoplasty Gathering organised by Dr Blønd and colleagues. Patients, having received the surgery, were interviewed, and shared their highly positive experiences. The fact that the technique is safe and reproducible and has no serious complications makes it a fantastic choice for patients and surgeons alike.

Personal Response
What do you envisage for the future of arthroscopic surgery? Do you believe a similar technique can be used for joints other than the knee?
<> I don’t see the arthroscopic trochleoplasty technique used in other joints, however I see that the technique can be improved by robot surgery. The indications might be extended to include patient with only light or medium trochlear dysplasia.