Serious illness decision-making:
How do you plan for uncertainty?
More than 2 million individuals around the world have now tested positive for COVID-19. While many people recover, or do not even realise that they are infected, approximately 5% become critically ill and must be cared for on an intensive care unit. A study from Seattle suggests that 50% of mechanically ventilated COVID-19 patients die. As of 17th April, the death toll has risen to almost 150,000.
With COVID-19 spreading at such an alarming rate, it causes much anxiety around the impact this serious illness may have on you or your loved ones. However, early discussion and preparation for the occurrence of serious illness can help reduce this anxiety.
For example, if you were to become seriously ill with COVID-19, the doctors will speak to you and explain what is going on and how they might treat you. But most people who are seriously ill are unable to think properly or speak. If this happens, doctors will usually turn to your substitute decision maker – this is usually a close family member or friend who would make healthcare decisions for you if you were not able to. These people feel tremendous stress when called upon to make these life and death decisions if they have not previously talked to their loved ones about their wishes.

To reduce this stress, some people might have an ‘Advance Care Plan’ (ACP) in place. Traditionally, these ACPs have focused on end-of-life or terminal care plans. Unfortunately, those plans are not necessarily suitable for the situation we are currently faced with as a result of COVID-19; planning for death under conditions of certainty (like when you have end-stage cancer) is not the same as planning for serious illnesses with uncertain outcomes (like COVID-19 pneumonia).
To combat this problem, Dr Daren Heyland, critical care physician, Professor of Medicine and Epidemiology at Queen’s University, Canada, and creator of the Plan Well Guide (https://planwellguide.com), is urging everyone to start preparing for serious illness, using an approach called ‘Advance Serious Illness Preparations and Planning’ (ASIPP).
Planning for death under conditions of certainty (like end-stage cancer) is not the same as planning for serious illnesses with uncertain outcomes (like COVID-19 pneumonia).
Advance serious illness preparations and planning
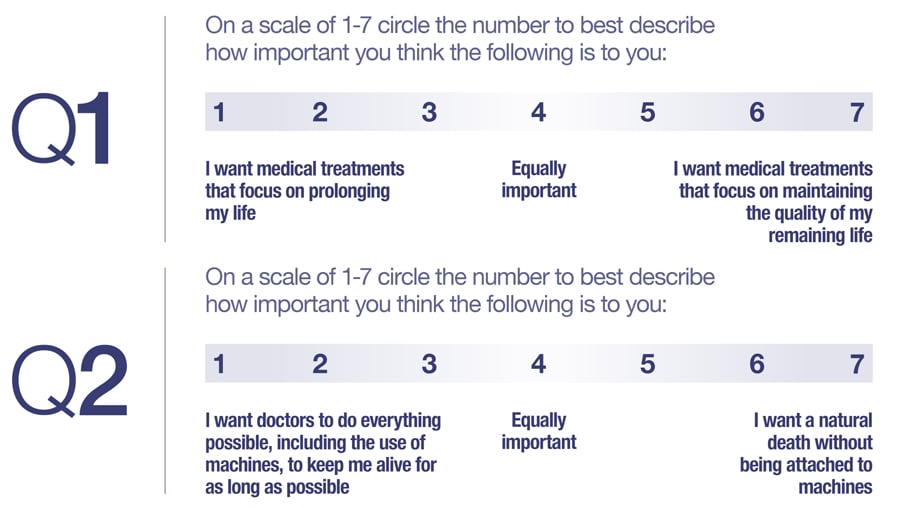
The current clinical approach of asking patients open ended values statements, like “What is important to you?” is inadequate as it doesn’t highlight the ‘trade-off’ or conflict inherent in the person’s answer, and the process of how the person’s answer translates into medical decisions is non-transparent and irreproducible. The rationale behind ASIPP is that doctors are able to use specific questions that better highlight these trade-offs and make transparent the links between patient values and available medical treatments that may be used to treat serious illness in the future. An example of the type of question is, “Are you the kind of person who wants medical treatments to focus on the quality of your remaining days or to focus on prolonging your life, for as long as possible?” or “Are you the kind of person who prefers a natural death or are you willing to accept the use of machines, such as breathing machines, to prolong your life, for as long as possible?” The answers to these questions help doctors make a decision that aligns with patient values. If the patient values treatments that focus on prolonging life and is open to making use of machines, then this suggests to the doctor that they should consider all possible treatment options for prolonging life in this patient. In contrast, if a patient values quality of life and doesn’t want machines at the end, then the medical treatments should focus on ‘comfort measures only’.
Alongside this, there is a need to find a balance between patients’ wishes and what is medically appropriate or indicated. The role of Plan Well Guide is not to enable patients to make medical decisions independently, like advance directives or living wills; but rather to prepare them to be able to articulate their authentic values and informed treatment preferences, so they are prepared to make decisions in collaboration with their doctors.
Providing the relevant information about treatment and outcomes is difficult when we do not know much about the condition. One problem we have when faced with COVID-19 is that we do not yet know the long-term health outcomes for patients who survive COVID-19 pneumonia. Therefore, it is more important than ever to have ASIPP discussions that consider this uncertainty. This is especially poignant as survivors of other prolonged critical illness experience significant impacts on day-to-day life, and a reduction in quality of life. This is something many older people don’t want to endure.
The Plan Well Guide
Patients should receive medical care aligned to their values and treatment preferences. However, the current approach of eliciting values and preferences is either absent or inadequate. How can these values be communicated when a patient is admitted to hospital? Most people do not deal well with decision-making under conditions of uncertainty, especially when it comes to their health; thus, there is a greater chance that people will make decisions they would not make under different circumstances.
Tools designed to guide decision-making have been shown to lead to improved knowledge, reduced conflict and increased likelihood of aligning treatment with patient values. Alongside this, there are also benefits for healthcare professionals. Recent work done by Dr Heyland investigated the efficacy of the Plan Well Guide in three Canadian medical practices. He found that using this tool reduced the time it took doctors to achieve medical care planning decisions with patients, as well as reducing decisional conflict for patients. Furthermore, the Plan Well Guide has been shown to increase patient knowledge of medical decisions, increased their confidence in discussing ASIPP with healthcare professionals and helped them clarify their values.
Key features of the Plan Well Guide include its ability to discriminate between planning for terminal care and planning for serious illness and an explanation of how clinicians make medical decisions during times of uncertainty. It also incorporates useful videos, such as the impact of CPR on survival rates and scripts to guide clinicians through difficult conversations with patients and family. Moreover, it includes contact details for health advocates, people who have health and social-work backgrounds and who can walk people through the ASIPP process, along with testimonials from users who have had success with the tool.
The role of Plan Well Guide is not to enable patients to make medical decisions independently, but rather to prepare them to be able to articulate their authentic values and informed treatment preferences.
The role of healthcare professionals
A survey of doctors from multiple centres identified barriers to goals of care discussions. These included the patient and/or family struggling to accept a poor prognosis, to understand limitations and complications of medical treatments, and disagreement between family members about what the goals of care should be.
The Plan Well Guide was thus designed to overcome these barriers and better prepare patients to discuss their overall goals of care. To facilitate this, the tool includes useful resources such as the creation of a “Dear Doctor” letter, which can be shared with the appropriate clinicians by the patient and their family.

Dr Heyland recommends that clinicians should encourage the decision maker, whether this be the patient or a family member acting in their best interests, to research the tool independently, before bringing their thoughts and feelings back for discussion with the healthcare professional responsible for the patient’s care. This does not always have to be a doctor; if another healthcare professional engages more successfully with the patient, then they can provide the appropriate support. When you do not have the luxury of time to send the patient and their substitute decision maker away to work through the planning process online by themselves, there is a worksheet that healthcare professionals can use to make decisions in the moment that helps clarify the values and makes transparent the decision-making. This worksheet for healthcare staff to make ‘in the moment’ decisions with Plan Well Guide naïve patients can be accessed through the Plan Well Guide (https://planwellguide.com/for-health-care-professionals/).
Conclusion
With the increase in COVID-19 related anxiety and uncertainty about the outcome if you do become ill, it is more important than ever to plan for future medical care. Doing so may reduce anxiety about getting COVID-19 because decisions will be in place regarding the medical care you wish to receive, and your family member advocating for you, if you are too sick to advocate for yourself, will be better able to represent you.
The Plan Well Guide aims to provide people with a more robust, reliable and relevant tool, so they are able to successfully establish values which need to be considered in the context of possible treatment options used during times of serious illness and uncertainty. It is free and provides tools and resources for patients and healthcare staff alike. Dr Heyland’s take home message: “You need to do your ASIPP ASAP!”

Personal Response
Taking a top-down approach, what can healthcare systems and health researchers be doing to encourage more frequent discussion about serious illness preparations with patients?
<>The goal is to get people coming into clinical decision-making more ‘prepared’. Thus, system leaders need to figure out how to embed these type of decision aids into the health care systems and clinicians need to ‘nudge’ or ‘prescribe’ to their patients that they engage in these preparatory activities (like going through the planning process on the Plan Well Guide) before the clinical encounter in which they have to make a decision about the type of care that is right for this patient.