Striking the balance between cost containment and high-quality care
Professor Karl Swedberg at the University of Gothenburg, Sweden, collaborated with a consortium of experts to produce a roadmap on cost containment for healthcare in the EU. The roadmap included ways to model proposed changes to see how they would impact on factors such as person-centred care and health promotion. The group’s work will help develop healthcare systems that offer the highest quality care to populations while ensuring that money and resources are used effectively.
Cost containment is a crucial part of healthcare costs. With healthcare costs increasing, it is important to manage this while still providing high-level, equitable care to individuals.
The European Council has agreed on specific healthcare-related values that need to be upheld by member states. These include universal access to good-quality healthcare, equity, and solidarity. However, these values must be considered within financial constraints, as in some countries overspending on healthcare costs may lead to health inequalities or shortfalls in other areas of spending.

Costs are already rising, with an increase from around 8% to 10% between 2000 and 2009, and these are likely to continue to increase, especially in view of the COVID-19 pandemic. Due to these costs, the Council also highlighted the importance of ensuring healthcare systems are financially viable.
Professor Karl Swedberg at the University of Gothenburg, Sweden, was part of a cross-disciplinary consortium of experts who aimed to produce a roadmap explaining how costs can be managed alongside improved healthcare provision.
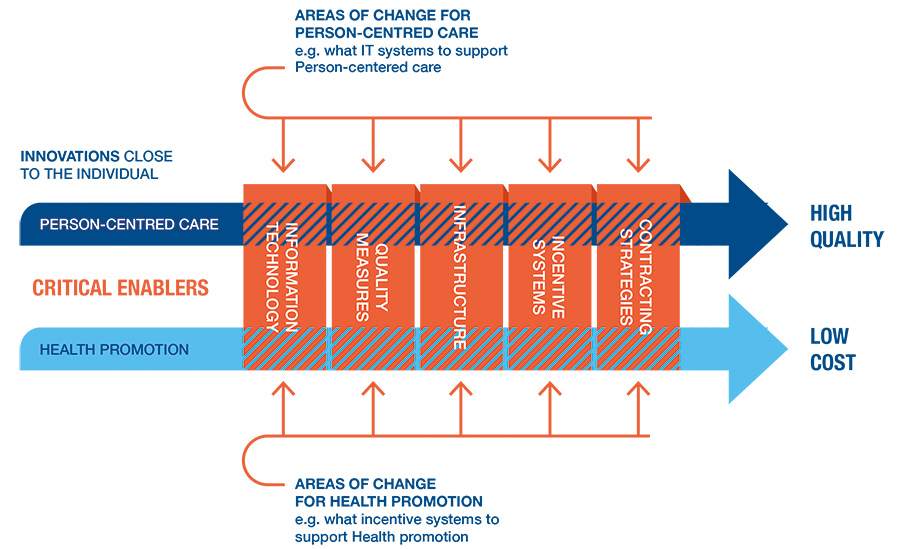
The roadmap was developed and tested through a project called COST-CARES that involved 28 European countries. Previous work from a similar project, the WE CARE roadmap, identified two main areas that drive the roadmap: person-centred care and health promotion.
Overspending on healthcare costs may lead to health inequalities or shortfalls in other areas of spending.
Professor Swedberg also explains that five critical enablers must be considered, including information technology, quality measures, infrastructure, incentive systems, and contracting strategies. These enablers move away from an individual level to consider broader factors that may influence the cost and quality of healthcare.
Drivers for change
Person-centred care (PCC) is a form of partnership between patients, their families and carers, and the team of health and social care professionals involved in their care. It is different from patient-centred care, which is often mentioned in healthcare, and focuses more on individuals once they enter medical services. PCC takes a more holistic view of a person’s resources, needs, preferences, and values. One example of PCC is provided by the World Health Organization (WHO), which adopts the view that individuals are both participants and beneficiaries of healthcare systems.

However, healthcare professionals and patients often have an unequal partnership, as clinicians may have more knowledge and control over a patient’s condition than the patient themselves. Despite this, patients have expert knowledge of their own needs. Working together, in partnership and agreement, ensures the most effective plan for patient care. As well as better outcomes for health, person-centred working also increases self-efficacy for patients, thereby further reducing the cost to healthcare systems.
In addition to PCC, health promotion is a major driver in the containment of healthcare costs. Targets for health promotion campaigns are usually conditions which could be avoided through lifestyle changes, such as high blood pressure, diabetes, and obesity. However, health promotion assumes that individuals have the freedom to make choices relating to their health, which may not be possible in food deserts (areas with poor access to a variety of nutritious food) or areas of poor socioeconomic status. Therefore, health promotion must also be enabled by higher governing bodies.
One crucial part of health promotion is empowerment or enabling individuals to take control of their own health. This overlaps with PCC, and Professor Swedberg emphasises the need for tailored approaches for each individual based on barriers, facilitators, and their wider environment.
Health promotion has a key role in containing healthcare costs as it represents a way to keep populations in better health and reduces healthcare costs.

Facilitators and enablers
As well as factors that drive cost containment, it is essential to consider what enables these changes to be made. For example, information technology offers great potential for increasing efficacy of care through automated systems, digital healthcare, and collection of patient data. Exploring data collected by these systems may provide insights into health at an individual and at a population level, highlighting where changes are most needed or would have the biggest impact. On the other hand, these systems can be costly and present challenges when considering information security and privacy.
Quality measures are tools used to monitor and assess the quality of healthcare processes. They play a vital role in cost containment as researchers must be able to quantify outcomes, such as patient-related outcomes, cost, and safety.
Contracting strategies are required to set out an agreement between different partners in a healthcare system. This may vary between countries, depending on population health needs, local labour costs, and patient expenditure.
Alongside contracts, a high-quality healthcare system also requires the infrastructure to function correctly and at full capacity. Integrating different areas of the infrastructure will result in cost savings and more efficient use of resources. Changes to healthcare systems cannot be made effectively without the underlying infrastructure and care contracts to support them.
Finally, what may incentivise healthcare workers to make a change or meet outcomes? Professor Swedberg points out a lack of evidence in this area, with many incentives based on financial outcomes, something that would also need to be considered in cost containment.
The COST-CARES project
The COST-CARES project aimed to continue the work of the WE CARE study, working towards an integrated approach between researchers, industry, healthcare professionals, policymakers, and patient representatives.
The main aim of COST-CARES is to establish ways to implement PCC as well as a framework to simulate, evaluate, and review the impact of PCC and health promotion in different countries.
Being able to test these changes in a laboratory setting means that there is a consistent approach taken to cost containment, in which data can be assessed and documented to inform other countries and future interventions.
Intervention strategies that account for the interplay between person-centred care, health promotion, and different enablers will be the most sustainable and effective options.
Professor Swedberg explains that it can be challenging to develop and test care models. Healthcare systems are complex, and the model must account for the needs of multiple stakeholders. It can also be difficult to exactly match the real-world interactions between a large number of interacting disciplines, and lab-based care models are often a simplified version of these relationships. There is a lack of evidence to show how these models can be upscaled to meet the needs of the population and healthcare system.
Testing different combinations of any number of the five enablers mentioned previously (technology, quality measures, infrastructure, incentives, and contracting) allows researchers to explore how the various enablers would improve PCC and health promotion. If a model can be found that clearly provides the greatest improvements in PCC and health promotion while containing costs, then ways to overcome barriers and implement the model can be developed. As each laboratory that will be testing these strategies will differ from others in terms of its location and social environment, there will be different models required for different settings.

The researchers concluded that existing lab models need to be expanded and developed to account for many complex interactions. One way this can be achieved is through the use of programme theory, a series of explanations that are able to link together different parts of a model to produce specific outcomes, which can then be used to inform interventions and other models of cost containment.
Finding the balance
Professor Swedberg concludes that cost containment of future healthcare needs to be addressed in a planned and logical manner. This should include a framework to test different models of drivers and enablers in different European countries.
COST-CARES is already examining how this may be achieved at different levels; this includes testing the intervention itself and the professionals and patients involved, the context in which this would occur, such as a hospital or health centre, and the broader picture, for example the types of healthcare policy and funding processes that are specific to individual European countries.
Intervention strategies that account for the interplay between person-centred care, health promotion, and different enablers will be the most sustainable and effective options. Alongside this, collaborative working between stakeholders is key to testing cost containment of healthcare while maintaining or improving quality of care.
Personal Response
What first inspired you to work in this field?
Having worked in clinical medicine for 50 years, I have experienced that technology development has left the patient’s opinion behind. The concept of person-centred care makes the patient a partner in care. The importance of this partnership has been tested by our group in more than 20 controlled trials. It was then important to move ahead in an international setting which led to WE CARE, followed by COST-CARES. The next step would be to test what is suggested in COST-CARES, but this has not been done yet.