Meltdown Moments: When the emotions of perinatal mums are out of control
The period from conception through the second year of a child’s life is a unique and critical time in human development, and experiences during this time can have a lifelong impact. In this period – sometimes referred to as the first 1000 days – babies’ brains are developing at dizzying speed. As they explore the world, their attachment to their primary caregivers is key in helping them navigate and appropriately respond to others. These early days lay the foundations for lifelong emotional and social wellbeing and it is increasingly accepted that many psychiatric conditions have their basis in very early childhood.
Associate Professor Anne Sved Williams, an expert in mother and infant mental health at the University of Adelaide, Australia, aims to improve understanding of and advocacy for new mothers living with psychiatric conditions. Her key focus is those who experience borderline personality disorder (BPD) or significant ongoing emotional dysregulation (those who nearly fulfil the criteria for BPD). Through her work she hopes to improve the quality of life for mothers with these conditions and to maximise the chance of a positive life course for their infants. Together with a team of psychologists and other mental health professionals, Assoc Prof Sved Williams is committed to finding out more about how BPD affects women and babies and how common it is in society. Their ultimate goal has been to design approaches to help these women, their infants and their wider families manage their condition.
The 2020 coronavirus crisis and its accompanying strict lockdown measures mean her work is now more relevant to many families with small children around the world: Increased pressure is being put on family life as families grapple with being confined to small spaces, dramatic economic consequences, isolation, grief and fear of infection.

Borderline Personality Disorder
BPD is one of several personality disorders – conditions that affect the way that people think about and relate to both themselves and to others. People living with BPD often find it difficult to control their emotions and behaviours and, as a result, act very impulsively. A common component of BPD is emotional dysregulation (ED) that consistently disrupts how people live their normal life. People with BPD typically feel worried about abandonment, have very intense emotions, find it hard to maintain friendships, and get angry very quickly. Risk taking, paranoia and suicidal thinking and behaviours are common. Many with BPD have a history of childhood trauma including sexual, emotional or physical abuse, but more recent theories suggest that parenting styles may also have a central role in the development of BPD.
BPD was found to be more prevalent than better-known conditions including post-partum psychosis and bipolar disorder.
How common is BPD in new mums?
BPD is much more common than most of us might assume with as many as 6% of people attending primary healthcare having this condition. The Sved Williams group is based in Helen Mayo House, a mother-baby inpatient unit for mothers with psychological conditions in Adelaide. A study led by Chris Yelland from the group, showed that almost a quarter of mothers in the study were diagnosed with BPD, and almost half the admitted women showed features of BPD on a self-report measure. BPD was found to be much more prevalent than better-known conditions including post-partum psychosis and bipolar disorder.

Motherhood is a testing time for anyone but can trigger mental illness in those living with a mental health condition. Sleepless nights, body changes, birth recovery, impact on relationships and the constant demands of an infant can exacerbate existing mental health conditions. Many women with previously undiagnosed BPD or ED who are normally able to manage their condition find that they no longer can. They experience low mood, suicidal thoughts, angry outbursts and difficulty in caring for their babies. The infants are often unsettled and may have additional issues with feeding and sleeping. Consequently, the relationship between parent and child is compromised: a mother may experience difficulty relating to her baby and to her own emotions. The situation can rapidly deteriorate.
Assoc Prof Sved Williams and her team recently carried out a study exploring how mothers with BPD respond to their baby’s crying. Common themes that emerged from the study showed that women with BPD typically experienced intense emotional pain and cognitive chaos and often mentioned suicidal and infanticidal thoughts in response to the crying. These results highlight the need for urgent intervention.
An overlooked condition
Assoc Prof Sved Williams – a former director of Helen Mayo House – believes that BPD is often under-diagnosed and under-recognised, particularly compared to postnatal depression, leaving psychological therapies that could help patients out of reach. Given the high prevalence of borderline personality disorder and emotional dysregulation identified in new mothers, there is a pressing need to do more to help these women and ensure the wellbeing of their infants.

Intervening to help mum and baby
Given the surprisingly small number of interventions for perinatal BPD and the absence of those which involve therapy with both mother and baby, the team has embarked on a new approach to tailor psychotherapy interventions specifically for this troubled group. A key aim of their initial research was to ensure mothers and babies access the program as early as possible. Early intervention comes at a time when interactional patterns are becoming established in the mother-baby relationship and can potentially prevent damaging behaviours becoming entrenched.
The team has embarked on a new approach to tailor psychotherapy interventions specifically for mother-baby relationships.
The new intervention is based on dialectical behaviour therapy (DBT) – a type of psychotherapy developed by Dr Marsha Linehan that aims to help people who experience overwhelming emotions accept their emotions, change harmful behaviours and improve close relationships. Mother-infant DBT (MI-DBT) is adapted to focus on the relationship between mother and baby. Taking the components of DBT, it involves 24 group sessions over 24 weeks, comprising elements including distress management therapy and intense education on infant development and socialisation. A pilot study has shown very promising results, with improvements in mood, reduced anxiety, better emotional regulation and some improvement in parenting. Scores on a parent-baby interaction index showed some improvement for a majority of the pairs. An analysis of a larger trial with 50 mother-baby pairs as yet unpublished confirms most early results for mothers.
Meltdown Moments
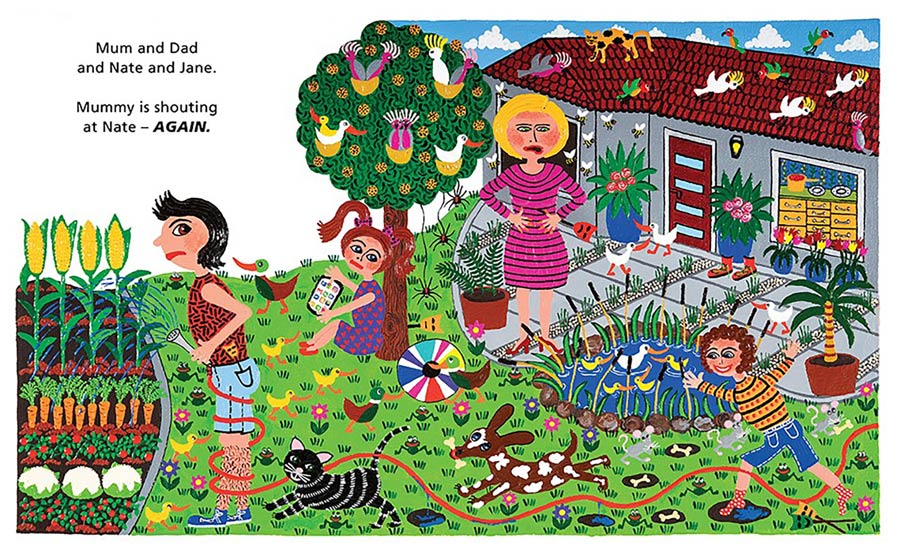
Assoc Prof Sved Williams is committed to improving understanding of perinatal emotional dysregulation and its more severe manifestation, BPD. She has recently published guidelines with Professor Gisele Apter, Chair of Child and Adolescent Psychiatry, Groupe Hospitalier du Havre in France, aimed at general practitioners to help them spot troubling signs in infants. Improving understanding of BPD is also crucial within the family unit itself and could help families manage the condition. To that end, Assoc Prof Sved Williams has teamed up with illustrator Marie Jonsson-Harrison to create an innovative picture book, Meltdown Moments: Helping families to have conversations about mental health, their feelings and experiences. The book is available on Amazon and all profits go to the Women’s and Children’s Hospital in Adelaide. Families can read the book with their small children to help them to understand BPD/ED and encourage conversations about what the family might do to change things. Following the 16-page picture story, Assoc Prof Sved Williams has provided several pages of psycho-educational material about BPD, emotional dysregulation, parenting and getting help.
Time is of the essence
Infants’ needs are urgent and timely interventions are essential to ensure a better life-course for infants and mothers. Early indications from the MI-DBT trial showed that there is excellent retention in the groups with documented benefits for both mother and infant. Community-based referrals and word-of-mouth interest in the study and group therapy have both been exceptionally high leading to a much wider expansion of the program in South Australia, with promising results from these community-based groups as yet unpublished. This uptake is encouraging but also underlines the urgent need for program refinements, better resources in places other than Adelaide and help for these mothers and babies living in the community. Like all parents, mothers with BPD want to do the best by their children and commonly speak of their concern about passing BPD to their children. Assoc Prof Sved Williams’ work makes the crucial early intervention possible, helping to improve these women’s mental health and secure their infant’s lifelong emotional wellbeing.

Personal Response
Ideally, how should your therapy be incorporated into existing therapy methods for BPD?
<> Mothers really appreciate working with other mothers in a similar life situation so we run groups in our unit where the mothers meet and their infants are provided with care. This also allows for the therapists to help the mothers with separations and reunions as the mums head to the group and back from it. They spend the last 20 minutes of group time with their infants present, practising with their infants what they have just learned in the skills-based DBT group, so the focus is all on parenting.
Is there an element of your work you find most enjoyable?
<>I love knowing we are offering something very unique which certainly helps the mothers and may also help the life-course of their infants, and perhaps their partners too.
