Why do women experience more chronic pain than men?
Chronic pain is poorly managed by current healthcare systems, with limited treatments. However, little is known about chronic pain, especially in autoimmune diseases. Dr Gurmit Singh and colleagues at McMaster University, Canada, have investigated whether chronic pain should be considered an autoimmune disease and why chronic pain is more common in women. They have identified various explanations as to why women may experience more pain than men and have stated that with these sex differences in mind, more could be done to develop new and improved treatments for chronic pain.
Chronic pain is a serious health condition and a significant cause of disability; as such, it dramatically reduces the quality of life of those suffering from it. Unfortunately, chronic pain is poorly managed by current healthcare systems. From 2015 to 2018, 10.7% of adults in the US used prescription pain medication to manage their symptoms. However, existing pain medications that treat chronic pain, like opioids, are only partially effective in treating symptoms and are heavily associated with opioid-related overdoses and even death. Despite this, there has been little development of more effective treatments to manage chronic pain.
Chronic pain is usually defined as pain that lasts longer than three months. It’s caused by neuronal activation and the body’s inability to repair damaged nerves. This is commonly seen in autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus (SLE), and osteoarthritis. Common to all these diseases is the immune system mistakenly attacking the body’s healthy cells – this is referred to as ‘autoimmunity’.

Dr Gurmit Singh, a professor and associate chair of research in the department of pathology and molecular medicine at McMaster University, Hamilton, Canada has focused his research on why women experience more chronic pain and autoimmunity than men. In a recent paper, Singh discussed hypotheses as to why these sex differences exist and highlighted how the immune and nervous systems work in tandem to coordinate chronic pain in autoimmunity.
Chronic pain and autoimmunity
Chronic pain is usually paired with autoimmunity due to the bidirectional relationship between the immune and nervous systems; interactions between the two are crucial in initiating and maintaining pain. Nociceptors are receptors in the body’s periphery which detect tissue damage directly, or indirectly through chemical signals released from tissue damage. However, dysregulation of signals between these two systems can lead to heightened responses from nociceptors.
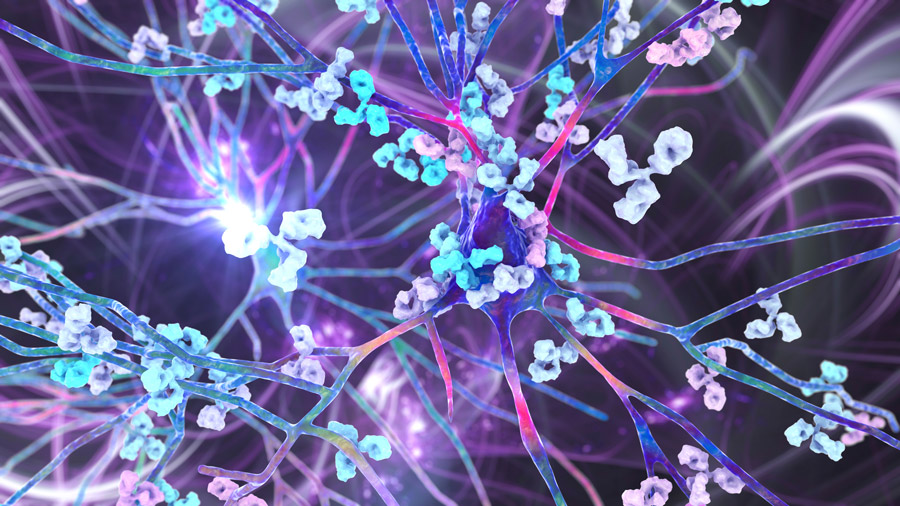
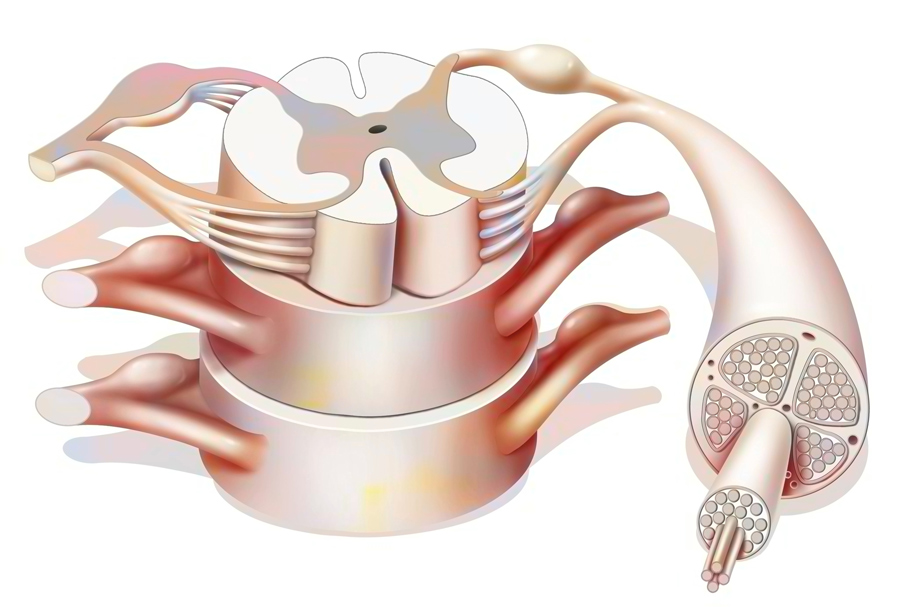
One of the most common features in autoimmune disease and proposed mechanism to describe chronic pain is autoantibodies, which are antibodies that attach to self-antigens – molecules released from healthy tissues – and destroy them. Antibodies subtypes like IgG and IgM are commonly responsible for autoimmunity. Autoantibodies influence the excitability of neurones by activating the complement system, which is a cascade of events that ultimately results in cell death through the recruitment of immune cells, inducing tissue damage. Autoantibodies do this by directly signalling at nociceptors expressing Fc gamma receptors, which are key in the immune response, or binding directly to nociceptors and disrupting ion channels. Feedback from the nociceptors in the periphery is thought to act via the dorsal root ganglion (DRG), which is a bundle of spinal nerves that detect pain, causing a cascade of events resulting in hyperexcitability of neurones, chronic pain, and inflammation. The DRG has an established role in chronic pain. In cases of nerve damage, nociceptors can become activated in response to non-threatening stimuli like stroking the skin.
Pain in autoimmune diseases is usually due to localised or systemic inflammation at the site of tissue destruction achieved through complement activation or by the release of pro-inflammatory cytokines. Studies have correlated high levels of complement proteins with nerve injury and disease progression in patients with rheumatoid arthritis. Singh suggests that the similarities between inflammation and autoantibody-mediated pathology provide support for chronic pain being regarded as an autoimmune disease.
Sex differences in chronic pain
Interestingly, women are more likely than men to experience chronic pain, autoimmunity, and autoimmune diseases paired with chronic pain. Conditions like Sjogren syndrome, an autoimmune disease affecting the eyes and mouth’s ability to produce tears and saliva, and SLE, an autoimmune disease which attacks many tissues and organs, affect women nine times more than men. Studies have revealed a strong genetic component in contracting these diseases – but why are women more likely to suffer from these autoimmune conditions?
By identifying components of the immune system which respond to the placenta, female-specific treatments against novel genetic targets could be developed.Singh explains that biological sex is an essential factor overlooked in autoimmune diseases, which could provide an explanation for autoimmune mechanisms in chronic pain. Conditions like back pain, migraines, and osteoarthritis are experienced significantly more in women than men, with the most significant difference between men and women being between the ages of 20-30 and declining after menopause. Reports suggest that there is a sizeable hormonal influence over the amount of chronic pain experienced. In a questionnaire study completed by 45,000 people in 16 European cities, chronic pain is consistently reported more in females than males, accounting for important factors like age.
However, Singh emphasises this is not true for all conditions where chronic pain is experienced. Diseases like neuropathy associated with diabetes, which is a condition which causes nerve damage resulting in weakness, pain, and tingling in one or more body parts, occur at the same rate in both sexes. It is important to note that there is unlikely to be a singular pathway that can solely explain sex differences in chronic pain, as many risk factors influence autoimmune diseases.
Pregnancy compensation hypothesis
The pregnancy compensation hypothesis suggests that immune system changes during pregnancy are ancestrally inherited. Singh and others speculate that pregnancy has shaped the evolution of the female immune system, forcing selective pressure on genes located on the X chromosome to provide optimal regulation of immune responses and to prepare their placenta for an immunologically-challenging environment. The female immune system ensures the developing foetus is not rejected, as the foetus is seen as a foreign body. This weakens the immune system, making pregnant women and the developing foetus susceptible to pathogens. The female immune system is believed to be primed to search for pathogens throughout its life and is often overprepared and overreactive to unthreatening stimuli like the body’s cells and tissue, resulting in autoimmunity. By identifying components of the immune system which respond to the placenta, female-specific treatments against novel genetic targets could be developed to better manage and understand chronic pain and autoimmunity in women.
X chromosomes
In pregnancy, during the embryo development in females, one of the two X chromosomes will become inactivated, rendering one X chromosome non-functional. X chromosome inactivation involves silencing genes; this inactivation has been associated with psychiatric disorders and some autoimmune diseases like SLE and thyroid autoimmunity. X chromosome silencing is achieved through epigenetic modifications (which are modifications made to the genes, turning them on and off due to environmental influences like smoking) or through the coating of the X chromosome by the protein X-inactive specific transcript (XIST). XIST attaches to the X chromosome and inactivates it. XIST is differentially expressed in immune cells in females and males, which is essential in coordinating the immune response. Women with XIST are more likely to experience chronic pain. Reports show that if normally inactivated genes on the X chromosome were to become activated, it could disrupt the immune tolerance in women and even cause autoimmunity.
Considering chronic pain as an autoimmune disease will increase the scope and potential to develop chronic pain therapeutics.The X chromosome has been associated with higher pain and post-traumatic stress rates in females than males. A study found that following a car accident, 40 genes from the X chromosome differentially expressed in females were associated with the later development of chronic musculoskeletal pain compared to those who recovered.
Testosterone and the Y chromosome
Unlike the X chromosome, all Y-linked genes are expressed. Current investigations are examining whether neural development in males could be related to Y chromosome gene expression or due to testosterone production in relation to the Y chromosome. However, Singh explains that gonadal hormones – hormones required for development – are as important in pain as the X and Y chromosome influence. Research has found that sex chromosomes and gonadal hormones influence nociception development in mice. Nociception refers to processing stimuli like tissue damage or temperature sensitivity by the central and peripheral nervous system, which activates nociceptors. However, the hyperexcitability of nociceptors can differ between sexes based on the hormone profile. It is widely accepted that testosterone is immunosuppressive, making it protective against autoimmune disease. The male diagnosis of Klinefelter’s syndrome, which causes a lack of testosterone due to having three sex chromosomes (XXY), is associated with an 18-fold increased risk of SLE.

Interestingly, males may also have a biological content within their Y chromosome, making their immune system more resilient to pain. Evolutionarily, men are hunters and gatherers and may have developed a mechanism to suppress pain to carry out their required duties. However, Y-linked genes and testosterone associated with chronic pain will be of interest in the future to help us understand their role in autoimmunity.
What now?
Despite the known contribution of sex hormones in autoimmunity and chronic pain, there is accumulating evidence that supports that immune-related conditions have a sex bias in children before puberty, too, emphasising the need to explore all possibilities to explain the sex differences in chronic pain better. According to Singh, deciphering the relationship between the nervous and immune systems and how autoimmune signalling pathways and sex differences contribute to pain is crucial for drug design and developing new effective treatments for managing chronic pain. It will allow us to treat females and males more effectively. After all, the body’s systems do not operate independently; they all interact and influence each other.
Singh strongly believes that considering chronic pain as an autoimmune disease could open new avenues to explore in terms of treatments and will increase the scope and potential to develop chronic pain therapeutics.

Personal Response
What inspired you to research chronic pain and how sex differences can influence the amount of pain experienced?Chronic pain is a major health issue worldwide. It causes morbidity and severely curtails quality of life. While pain is a symptom of a number of diseases in the acute phase of a disease, if prolonged, it becomes a chronic disease on its own. Chronic pain is experienced frequently by women. This dichotomy in pain experience between men and women was the impetus in my laboratory to examine sex differences. Furthermore, drugs used for pain management affect men and women with a varied efficacy.
Do you believe chronic pain should be classed as an autoimmune disease?
The frequency of chronic pain in women is similar to other autoimmune diseases. The common biomarkers in pain are associated with a heightened immune system, namely cytokines such as IL-6, TNF-Alpha, etc. Injury to nerves is associated with increased immune surveillance for repair. However, if the immune response is prolonged as in other autoimmune diseases, the symptom becomes a disease as in chronic pain. I believe we have circumstantial evidence to support the notion that chronic pain is an autoimmune disease. Having proposed a novel hypothesis, it opens an avenue to explore the possibility and provides novel targets for the treatment of chronic pain.
What has been your greatest achievement in this field of work?
Pharmacological examination of drugs in overcoming chronic pain in animal models provided a window of opportunity to examine their dimorphic response. This was observed with cannabinoids and opiates. With a novel hypothesis, we were able to focus on the interaction of the immune system and the nervous system. I believe these observations will lead to novel treatments for chronic pain. A paradigm shift in chronic pain research will result in enhanced quality of life.