New therapy offers hope for wound healing in severely burned patients
The human body has a remarkable ability to heal itself. Sometimes, though, the damage is just too severe, and even with the best medical care, the prognosis is poor. This has long been the case for patients with serious burns.
Third-degree burns – where the burn fully penetrates all three layers of the skin – are the most difficult to treat. These patients suffer severe pain and are at high risk of infection, leading to treatment with intravenous antibiotics, as well as other clinical complications. If the burn is extensive, the patient may require a skin graft – a therapy that has been used for decades. This process uses a thin layer of healthy skin from elsewhere on the patient’s body which is meshed and grafted to the damaged area. Unfortunately, this treatment is imperfect and does not always result in successful wound healing.

Split-thickness skin grafts
A type of skin graft commonly used in burn patients is called split-thickness skin grafting. This involves transplanting a thin piece of donor tissue, comprising the outermost layers of the skin: the epidermis and part of the dermis. The graft is usually taken from a part of the body that heals well, such as the thighs or buttocks.
The advantage of a split-thickness skin graft is that the donor site normally heals well within a few weeks, because the deeper part of the skin is left intact. However, there are some disadvantages. Only the outermost part of the skin is used, so the wound site does not recover its full function. Split-thickness skin does not contain sweat or oil glands, or hair follicles. So, although split-thickness skin grafts can effectively function as a barrier, they may not aesthetically match the surrounding skin, for example in colour or texture. There are also risks of graft failure, contraction of the donor skin and scarring.
Full-thickness skin grafts are also possible but leave a deeper wound that must be completely closed in order to heal and are limited by a 1:1 expansion ratio. For this reason, grafts must be relatively small and are not suitable for covering large wounds. Both full-thickness and split-thickness skin grafts have a failure rate of around 30%.
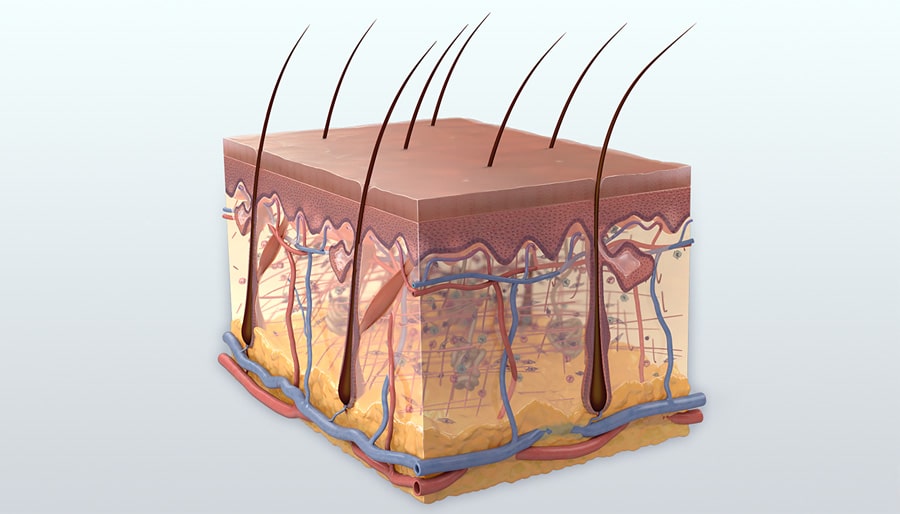
Skin is a complex biological organ, with roles in cell signalling, metabolism and protein synthesis.
A new option
PolarityTE has developed an innovative treatment, SkinTE™, for burns and other hard-to-treat skin defects, including wounds and traumatic injuries. PolarityTE is a biotechnology company that is focused on discovering, developing, and designing regenerative tissue products. SkinTE™ is a novel, first-of-its kind treatment. The advanced technique has the potential to eliminate the unfavourable results of traditional treatments, like split-thickness skin grafts.
SkinTE™, is an autologous homologous skin construct (AHSC). “Autologous” because the tissue comes from the patient’s own body, and “homologous” because the donor graft will perform the same function in the area to which it is applied.
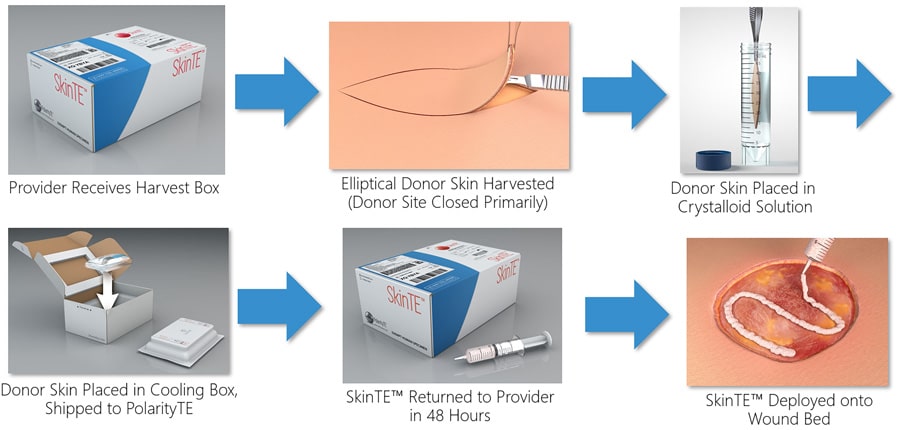
The company has established a seamless process for deploying SkinTE™. First, using a harvest kit provided by PolarityTE, the healthcare provider removes a small piece of healthy, full-thickness skin from the patient. Only a small sample of skin is needed to cover a large wound area, leading to minimal harvest-site morbidity. This differs from other methods which have been developed with a similar aim but use artificially manipulated homogenous cells. The skin harvest is packed in a sterile, temperature-controlled container. The sample is returned to PolarityTE’s laboratory and the tissue is processed into AHSC or SkinTE™. Once processed, SkinTE™ is returned within 48-72 hours to the healthcare provider in a deployment box. Once the affected area is cleaned and prepared, SkinTE™, contained within a syringe, is applied over the wound. The area is then dressed and treated akin to other types of skin grafts. Over time, SkinTE™ grows and expands to become full-thickness skin with a histology comparable to native skin. Throughout the process, healthcare professionals can communicate with a PolarityTE team of Clinical Science Managers. Treatment with SkinTE™ has been proven to regenerate skin with all layers, appendages and has even produced function such as sensation, sweat and pliability.
The development of SkinTE™ was inspired by recent research that shows that skin is more than just a barrier. Skin is a complex biological organ, playing major roles in cell signalling, metabolism and protein synthesis. It is also a crucial part of the nervous system, immune defence mechanisms and hormonal functions. This shows the importance of utilising full-thickness skin, with a complete complement of functions, to help heal wounds with a wide range of size and severity.
As well as burns, SkinTE™ can be used to treat chronic wounds, including diabetic foot and venous stasis ulcerations, acute traumatic wounds and amputation sites. It could also serve as a viable replacement of failed skin grafts, to replace scar tissue, and facilitate surgical reconstruction.

Promising results
SkinTE™ has already been used in a variety of clinical settings, ranging from intensive care units to wound care centres and outpatient clinics. PolarityTE is currently running multi-centred, controlled trials to compare SkinTE™ to current standards of care. Up to 16 centres in the US are expected to participate in each trial. In addition, several clinical trials are specifically comparing SkinTE™ to split-thickness skin grafts in burn patients. Two further trials are evaluating the new treatment when applied to diabetic foot ulcers and venous leg ulcers.
SkinTE™ has already produced very encouraging results. In one particular case, SkinTE™ was used to treat a patient who had suffered very serious burns in a house fire. The 45-year-old woman had burns to 75% of her body surface, including on her arms, legs and torso. She developed multiple complications, including septic shock and acute kidney injury. Due to the extent of the injuries, the patient had little healthy skin that could be used for conventional skin grafting.
SkinTE™ offers the potential for better treatment of extremely serious conditions and injuries.
A small sample of healthy skin was taken from the patient’s abdomen using the PolarityTE® harvest kit. The sample was processed into SkinTE™ at PolarityTE and applied to the patient’s wounds two days after the small donor sample was taken. SkinTE™ was applied to the burns on the patient’s legs. At the same time, split-thickness skin grafts were used to treat the burns on her arms, using skin taken from the front of her torso.
By six weeks after SkinTE™ was deployed, full epithelialisation (the spread and anchoring of epithelial cells over the wound) on the patient’s legs had occurred. This is the first step in the formation of new skin, where the new cells act as a barrier. By eight weeks, the patient was able to leave the hospital. At six months after SkinTE™ treatment, the regenerated skin on the patient’s legs had developed full function, as well as re-pigmentation and normalization. Unfortunately, the patient experienced contraction (when the graft shrinks) and irritation of the skin grafts applied to the wounds on her arms.

In this case, SkinTE™ was an effective treatment for a patient with extensive, full-thickness burns. SkinTE™ regenerated full-thickness skin, and developed pigmentation, improving the appearance of the affected area and ultimately, improving the patient’s quality of life. Like most cases, only a single application of SkinTE™ was needed.
A brighter outlook
The novel technology behind SkinTE™ may offer better treatment of serious skin defects, injuries and conditions. Dr Nikolai Sopko and his research team believe that SkinTE™ has multiple benefits, including the ability to improve the function of new skin and the reduction in healing time, which can ultimately lead to shorter hospital stays and improved healthcare economics. SkinTE™ removes the need for large skin grafts to be taken from other parts of the body, leading to minimal harvest-site morbidity. The treatment also avoids some of the complications often seen with traditional split-thickness skin grafting. If PolarityTE’s clinical trials continue to produce encouraging results, SkinTE™ could become established as a standard treatment for patients with serious burns, chronic wounds, and other debilitating cutaneous conditions.
Personal Response
Could the technology behind SkinTE™ be used to develop treatments for other types of injury or chronic condition?
<> The technology behind SkinTE™ is incredibly powerful, in part, because it harnesses our body’s remarkable ability to heal itself. Although skin has a tremendous capacity for repair, it has not evolved to deal with difficult-to-treat injuries such as complex traumatic wounds that can occur in motor vehicle accidents or chronic wounds that can occur with ageing and exposure to chronic diseases. The technology helps optimise the body’s healing potential to close these challenging wounds, and we expect to see more and more encouraging clinical results in these settings. – Dr. Nikolai Sopko

Thanks for this article on the potential use of SkinTE in third degree burns. By Gregg L. Friedman MD