Patients as partners in research – The challenges for researchers of patient involvement
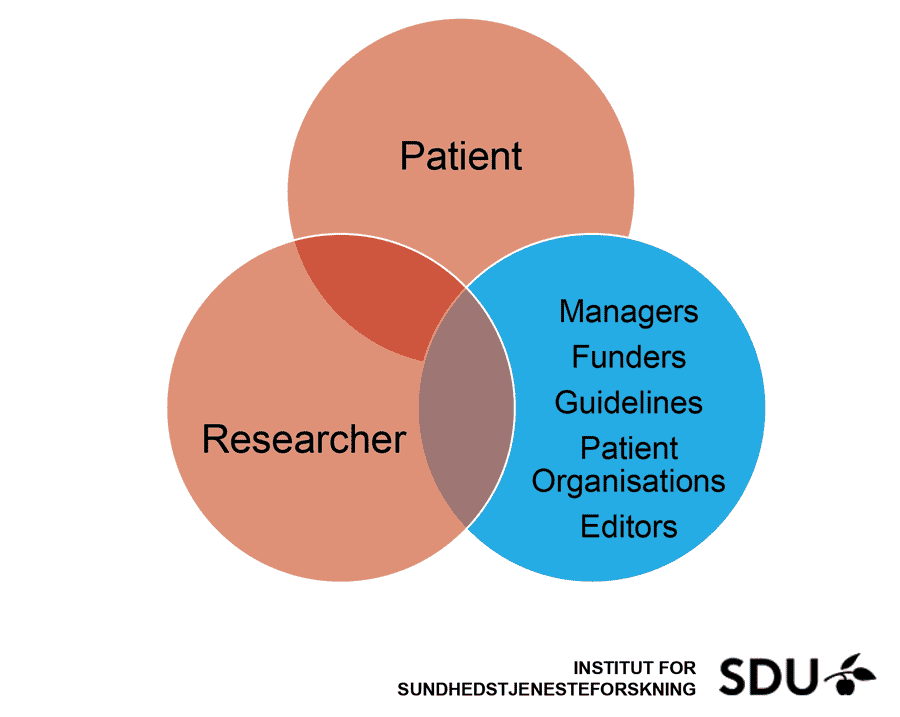
Patients are the benefactors of medical research. Yet, in the past, patients were regarded solely as passive objects in research-based development of new treatments and medicines. Research happened ‘for’ or ‘to’ patients, who played no active part in the research process. In recent years, however, there has been a shift in research practices. Patient involvement in research, also known as Patient and Public Involvement (PPI), is increasingly recognised as a valuable part of healthcare research. Rather than ‘for’ or ‘to’, research is now ‘with’ or ‘by’ the patient.
In PPI, patients are treated as research partners rather than simply recipients. The patient’s perspective on the research process is invited and can influence the direction taken by the research. Living with the condition being studied allows patients to offer unique and personal insights at all stages of the process, from planning and design of the study to communicating the results.

The challenges of PPI
While most researchers recognise the potential value of PPI, actually achieving this potential in practice can throw up many challenges. For many scientists, embracing PPI requires a shift in mindset. Some researchers believe that “science is for scientists”; perhaps understandably, a scientist who has dedicated years to their chosen specialism may struggle with the idea of sharing ownership of their work with a non-expert.
There is also the issue of identifying exactly what contribution is requested or expected from the patient: is it solely their experience of living with the disease or condition? Or could they offer more? How should patients be selected for participation – should the researcher aim for patients who are most representative of the patient population, or should those who are most willing or able to contribute be selected?
While most researchers recognise the potential value of PPI, actually achieving this potential in practice can throw up many challenges.
To better understand some of the challenges of PPI from a researcher’s perspective, and to seek solutions to potential problems, Prof Mogens Hørder and Prof Marie Konge Nielsen of the University of Southern Denmark scoured recent literature on the subject. Their aim was to answer three questions: what challenges and barriers do researchers face in PPI? What are some of the effects of PPI on well-established research practices? And what support do researchers need?
How does PPI affect the traditional research process?
Most scientific, medical and clinical research follows a well-established path. The traditional research process – which includes, for example, generating a hypothesis, designing a study, collecting data and analysing results – is robust and reliable. While incorporating PPI does not mean that this process will be overturned, it does mean that it might be approached in new ways.


In PPI, the patient’s perspective informs the research goals. When researchers are open to this, the view of the patient can steer the direction of the research, reveal overlooked issues, influence study design – and, crucially, ensure that the outcome is patient-centred. This has been particularly successful in arthritis research, in which patients have driven a new focus on quality-of-life measures such as chronic fatigue and sleep problems.
Prof Hørder and Prof Nielsen found that, according to many researchers, the potential of PPI varies according to the type of study. While PPI might be smoothly included in clinical research – in which there has always been patient involvement, even if only as research subjects – it is less relevant to basic research (which seeks to expand knowledge, rather than lead directly to a new treatment, for example).
While the success of PPI may vary from project to project, most researchers expressed a view that they are themselves changed by the process. For example, working closely with patients can force researchers to discuss their work in more accessible language, avoiding scientific jargon. As a result, researchers improve their ability to share their work with a
wider audience.

Prof Hørder and Prof Nielsen believe that researchers return to one question: “How will involving patients affect my project?” There is no single answer to this question. PPI will impact the research process of each project in a slightly different way. Nevertheless, PPI will likely reveal new issues or problems to consider – and perhaps solutions to investigate by research, as well.
PPI will likely reveal new issues or problems to consider – and perhaps solutions to investigate by research.
What support do researchers need?
It is clear that there is no ‘one-size-fits-all’ approach to incorporating PPI in a project. However, there are a few common factors that are important in successful PPI – and institutions should ideally have the proper support in place to allow researchers to address these points. First, patients should be involved at an early stage in the research process. This allows patients to understand and influence the aims of the project at the planning stage. It also enables them to have a sense of ownership over the work. Second, researchers should ensure that patients understand how and why their contribution is valuable. If addressed properly, these factors will strengthen the collaboration between patient and researcher.
While the researcher leads the project – and takes overall responsibility – it is important that the roles of each participant are clearly defined. This should be done as early in the project as possible, so that realistic expectations can be set. With the support of their institution, researchers could even consider written ‘job descriptions’ for both themselves and patient participants in order to clarify roles. Another possibility is for researchers experienced in PPI to guide and mentor those who are new to the task.

Both researchers and patients may need training in PPI. For the patient, this could cover the fundamental ideas of the research process: that research builds up knowledge that is based on data, that methodology is based on certain principles and theoretical assumptions, for example. For the researcher, training in communication – which could cover everything from discussing methods and results to chairing meetings – is likely to be beneficial. Researchers and patients could even participate in training together, which would help to build their relationship.
Finally, researchers agree that institutions should offer practical support for PPI. This could involve extra financial support – in meeting patients’ transport costs, for example – and help with budgeting. Institutions could also take responsibility for ensuring diversity in PPI: in the ethnic, cultural and educational backgrounds of participants.
The future: patients as partners
If PPI is to have value, the commitment of the researcher is key. There are many challenges for the researcher in successfully implementing PPI. Prof Hørder and Prof Nielsen believe that, as yet, these challenges have received little attention. To overcome problems and sustain the motivation of both researcher and patient participant, the support of the institution is crucial.
With the right support in place, researcher and patient will be able to work together in a constructive and mutually beneficial way. At its best, this collaboration will contribute to new scientific discoveries. A positive experience of PPI will lead the researcher to develop new skills and a richer level of experience, thereby enhancing the value of their future work.
Personal Response
In your opinion, what factor is most important in helping researchers to tackle the challenges of PPI?
<> Of major importance is to get started, to gain experience with PPI, to ensure feedback from patients and to share experiences among colleague researchers: “The researcher does not know what she does not know until she has asked the patient.” (Kristina Staley).