Unravelling the links between substance use and binge-like eating disorders
Binge eating disorder (BED) and substance use disorders (SUD) are characterised by maladaptive responses in the reward system of the brain. Dr Mary C Olmstead at Queen’s University, Canada, and Dr Katia Befort, University of Strasbourg, France, are using rodent models to explore how a part of the reward system, called the endocannabinoid system (ECS), affects the two conditions. They hope that their research will increase understanding of these disorders and lead to the development of novel treatments.
Binge eating disorder (BED) is currently the most commonly diagnosed eating disorder, affecting approximately 2.8 million adults in the USA alone. On a global level, close to 6% of women and 0.7% of men were diagnosed with BED between 2013 and 2022. The disorder is characterised by frequent episodes of excessive food intake within a short period, accompanied by a feeling of loss of control.

Existing evidence points to similar neurobiological mechanisms in BED and SUD. Both conditions are linked to emotional distress, and the people affected by these disorders often suffer from mental health disorders, most commonly anxiety and depression. Additionally, BED can lead to obesity, which is associated with serious health problems such as type 2 diabetes, hypertension, heart disease, and cancer.
The ECS contributes to the reinforcing effects of both drugs and food, identifying them as sources of reward for the body and increasing motivation to seek them out.Dr Mary C Olmstead at Queen’s University in Canada and Dr Katia Befort at the University of Strasbourg, France, are experts in the study of eating disorders. Their research suggests there is a shared etiology between SUD and BED that centers on dysfunction of the endocannabinoid system (ECS). Physiologically, the ECS influences the motivation for natural rewards, such as palatable food, sexual activity, and social interaction.
The role of the brain’s reward centre
As part of the brain’s reward centre, the ECS plays a critical role in functions such as learning, memory, emotional processing, and ingestive behaviours. It also contributes to the reinforcing effects of both drugs and food, identifying them as sources of reward for the body and increasing motivation to seek them out. Binge-eating episodes can involve any food group, although hyperpalatable foods that are high in sugar and/or fat are frequently chosen. Olmstead and Befort developed rodent models of binge eating to investigate changes in the ECS under a high-sugar and/or high-fat diet.
The team observed that in rats, this diet pattern led to excessive overeating. Analysis of brain tissue confirmed that there were changes in the expression of the ECS within brain-reward regions. In parallel, the researchers found that the diet also affected the dopamine system. Dopamine is a chemical messenger in the brain that activates the reward pathway. It instigates a feeling of pleasure as part of the brain’s reward centre and drives motivation to achieve the same reward sensation again.

Photo credit: Romain Bourdy
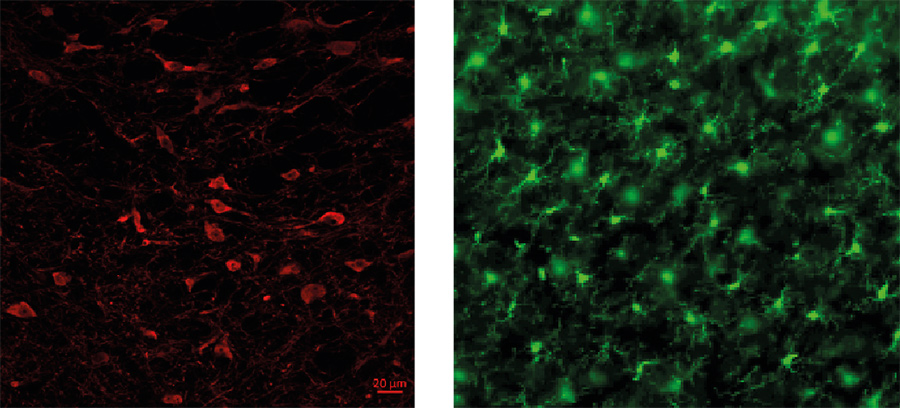
To explore similar phenomena in drug use, Olmstead and Befort investigated the effects of cocaine addiction on ECS expression in a rat model. This work highlighted a key role of the hippocampus, which primarily controls memory and learning, in cocaine-induced plasticity. More specifically, cocaine self-administration increased gene expression of cannabinoid receptors, which are molecules that modulate and fine tune how chemical signals in the brain are transmitted, altering the expression of reward-driven behaviours.
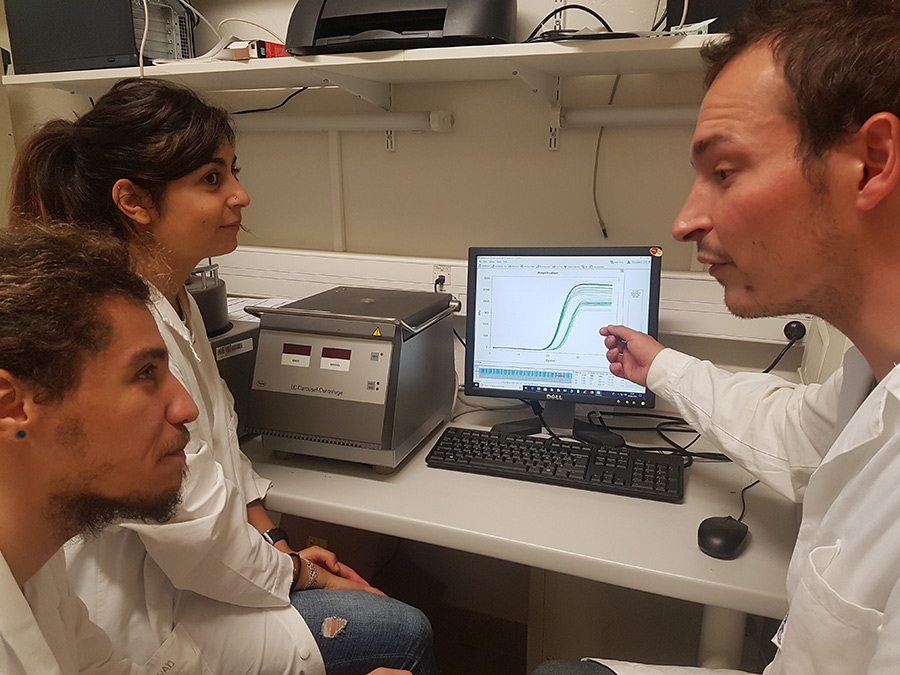
Photo credit: Romain Bourdy
Interestingly, the study also showed that cocaine can modify epigenetics and destabilise chromatin conformation, meaning that it can control which genes are turned on and off in this part of the brain. According to the researchers, these changes may cause a brain re-modelling that contributes to maladaptive behaviours in drug misuse. Continued drug abuse may therefore result in long-term changes in the brain, shaping behaviours that lead to addiction.
The attraction of hyperpalatable foods
In a first study to explore the contribution of the ECS to binge-like eating behaviours, rats were given intermittent (12-hour) or continuous (24-hour) access to high-sugar solutions and food. The time-restricted group showed excessive sugar intake within a short time period, that is, binge-like responses. Changes of ECS gene expression, as well as endocannabinoid levels, were observed in bingeing rats. In addition, blocking the cannabinoid receptors altered sucrose consumption, underlining the involvement of the ECS in palatable food eating. Interestingly, a similar binge-like eating pattern was observed in another study involving intermittent access to both high fat and high sugar (2h/day, 3 times/week). In these rats, a distinct profile of ECS expression was observed between bingeing and non-bingeing rats, highlighting changes specific to the eating behaviour.
In other studies, Olmstead and Befort established a binge-like model in mice. Only mice with intermittent access to sucrose (4h/day) developed binge-like behaviour, assessed as higher sucrose intake that escalated during the 1st hour of access. This effect was particularly magnified in mice with intermittent access to an artificially sweetened solution, which shows how little we understand about the impact of such sweeteners on hyperphagia, the act of overeating.
This study also examined the contribution of mu opioid receptors (MOP) to binge-like intake of sweet solutions. MOP play an important role in the hedonic responses to palatable foods so the researchers investigated whether high sugar intake would be altered in mice that were genetically modified to not express these receptors. Compared to mice with intact receptors, mice lacking MOP were less prone to develop excessive sucrose intake suggesting that feeling pleasure is an important component of binge behaviour. In another study, the research team showed for the first time that sucrose bingeing in mice modifies the positive reinforcing effect of alcohol. In other words, excessive sucrose intake changed how the animals experienced the pleasurable effects of alcohol. The same study showed that prolonged sucrose access, up to 8 weeks, exacerbated sucrose bingeing in female mice, and produced altered emotional states even in females that did not display bingeing behaviour. These findings broaden the understanding of behavioural alterations associated with sucrose bingeing, highlighting the need to investigate how this behavior interacts with addictive-like properties of drugs.
Photo credit: Romain Bourdy
Befort explains that genetically modified animal models have revealed a link between the ECS and eating behaviours, specifically addiction-like bingeing. Importantly, repeated episodes of bingeing or exposure to hyperpalatable foods may lead to reduced sensitivity of the reward system, meaning that individuals will consequently need more of these foods to get the same reward sensation they experienced previously. This reinforces a vicious cycle of increased food or drug intake seen with both BED and SUD disorders.
On the road to novel therapies
The work of Olmstead and Befort builds on the changes observed in the brain reward system associated with binge-eating behaviours. Their future investigations will involve cutting-edge technologies to further explore neural activity associated with addictive behaviors and to understand how anxiety is connected to food or drug bingeing. A growing number of studies highlight an important link between the digestive system and the brain in several psychiatric disorders, including BED and SUD.
Restricting access to palatable foods increases the likelihood of bingeing, a behaviour that is affected by brain reward mechanisms.In particular, the gut microbiota has been shown to play a major role in motivational processes, but very few studies have focused on understanding the brain reward mechanisms that mediate this connection. The team plans to investigate whether excessive and uncontrolled palatable food intake may induce adaptations in the gut microbiota that would be responsible for behavioral deficits, notably motivational ones, which would contribute to the development and/or maintenance of addictive behaviors. The team hopes that future discoveries will tell us more about the cause and effects of binge eating behaviours and the possible similarities/differences between BED and SUD.

It is clear that excessive eating and drug use bear immense personal and societal costs. A combination of pharmacology and psychotherapy appears to be the best option for patients. Understanding more about the mechanism behind these conditions will contribute to the development of novel therapies to treat eating and substance misuse disorders. Olmstead and Befort hope that their research will serve this purpose to help reduce the global health burden of BED and SUD, as well as improve the health and wellbeing of those affected by these conditions.
Personal Response
What inspired you to conduct these studies?We both worked in the field of addiction for many years investigating the impact of brain neuroadaptations on reward-related behaviours. The loss-of-control observed in BED is very reminiscent of a primary symptom of SUD, leading to notions of “food addiction” and skewing preclinical research towards the study of processes that would be common to both disorders. Indeed, similar neurobiological alterations in brain structures involved in reward-related processes could be the origin of, or at least contribute to, the maintenance of BED. Nevertheless, the dietary component of BED distinguishes it from SUD and points to the importance of better understanding which mechanisms are specific to BED.
How can the findings from rodent models be transferred to humans?
It is undeniable that animal-based research has contributed significantly to advancements in our understanding of molecular pathways involved in psychiatric disorders. In extending this work to BED, we recognised that establishing rodent models of binge eating was a critical step, allowing us to investigate specific neuroadaptations in this pathology and to correlate these changes with behavioural responses. Identifying similarities and differences between human and rodent binge eating will provide insight into the mechanisms of this complex disorder and contribute to advancing biomedical research and developing new therapeutic approaches to treat these devastating conditions.